Nerve growth factor, often called NGF, plays an important role in how the body senses pain. Because NGF levels are higher in painful joints, scientists thought that blocking NGF might be a powerful way to treat arthritis pain. This led to the development of anti-NGF monoclonal antibody drugs, such as tanezumab, which were designed to reduce pain by stopping NGF from activating pain nerves.
At first, the results looked promising. Many patients reported meaningful pain relief. However, over time, serious concerns emerged that greatly limited the use of these drugs in human medicine.
How anti-NGF drugs work
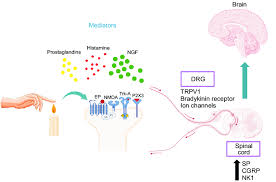

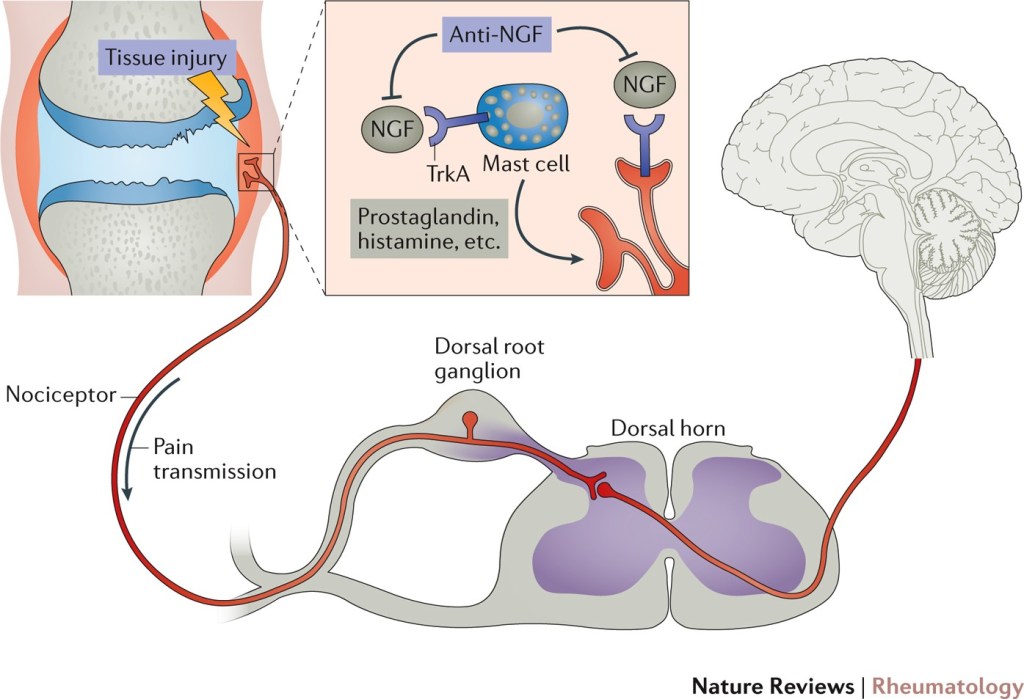
NGF helps pain signals travel from joints to the brain. Anti-NGF drugs block NGF from attaching to its receptor (TrkA) on pain-sensing nerves. This can significantly reduce pain, even when arthritis is advanced.
The problem is that pain is not just a symptom. Pain also protects us.
Major safety concerns in people
The biggest reason anti-NGF drugs are not widely used in people is safety.
Some patients receiving anti-NGF therapy developed rapidly progressive osteoarthritis. In these cases, joints deteriorated much faster than expected, sometimes within months. This damage was severe enough that some patients needed joint replacement surgery much earlier than anticipated.
Researchers believe this happened because pain was reduced so effectively that patients unknowingly overused already-damaged joints. Without pain acting as a warning signal, the joint continued to break down.
Increased risk when combined with other medications
The risk of joint damage was even higher when anti-NGF drugs were used together with common arthritis medications like non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs already affect joint biology, and the combination appeared to further increase the risk of joint failure.
Nerve and sensation side effects
NGF is involved not only in pain but also in normal nerve health. Some patients experienced abnormal sensations such as tingling, numbness, or burning pain. These nerve-related side effects raised additional concerns about long-term safety.
Regulatory decisions slowed progress
Because of these risks, the U.S. Food and Drug Administration (FDA) placed clinical trials of anti-NGF drugs on hold multiple times. Although some trials later resumed with stricter rules, the overall enthusiasm for these drugs declined.
Ultimately, regulators and researchers concluded that the risks often outweighed the benefits for most human arthritis patients, especially given the availability of other pain management options and joint replacement surgery.
Arthritis as a One Health disease
Arthritis is a classic One Health condition. It affects humans, dogs, cats, horses, and many other species, and it does so through remarkably similar biological pathways.
While dogs and cats are not humans, we are all animals and mammals. The fundamental structure of joints, the inflammatory mediators involved in osteoarthritis, and the development of pain pathways are highly conserved across species. NGF signaling, TrkA receptors, and nociceptive nerve function did not evolve separately in people and dogs. They are shared systems with shared strengths and shared vulnerabilities.
This means that lessons learned in human medicine are highly relevant to veterinary medicine, not because the patients are identical, but because the underlying biology is closely related. When blocking NGF led to unexpected joint deterioration in people, it highlighted a risk inherent to the mechanism itself, not just the species.
Why this matters for veterinary medicine
For veterinarians, the human anti-NGF experience provides important context rather than a direct comparison.
Dogs and cats do not make the same conscious decisions to push through pain in the way people do. However, animals can still increase activity when pain is reduced, particularly if their environment or owners encourage movement. This means the balance between pain relief and joint protection remains critically important in veterinary patients as well.
Another key difference is the treatment landscape. In people, joint replacement surgery is widely available and commonly used when arthritis becomes severe. In veterinary medicine, surgical options are far more limited, especially for elbows, shoulders, stifles, and spinal conditions. As a result, long-term medical management of osteoarthritis plays a much larger role in animal patients.
This is why veterinarians using anti-NGF therapies emphasize careful case selection, concurrent disease-modifying strategies (such as weight management, rehabilitation, and joint injections), and close monitoring for changes in mobility or joint health. Anti-NGF drugs should not be viewed as “pain blockers alone,” but as one component of a comprehensive arthritis management plan.
Importantly, the human experience reinforces that blocking pain does not treat the underlying joint disease. Whether in people or animals, therapies that reduce pain without supporting joint health may carry unintended risks if not used thoughtfully.
Take-home message
Anti-NGF monoclonal antibodies showed that targeting pain pathways can be very effective, but they also revealed an important lesson: pain exists for a reason.
Arthritis is a One Health disease, and the biology of pain is shared across mammals. While species differences matter, the similarities are significant enough that outcomes in human medicine should inform veterinary decision-making.
In people, concerns about rapid joint deterioration, nerve-related side effects, and regulatory hurdles have limited the use of anti-NGF drugs for arthritis. In veterinary medicine, these same lessons underscore the need for cautious, individualized use and a strong emphasis on protecting joint health alongside pain control.
Understanding why these drugs struggled in human medicine helps veterinarians apply them more safely, responsibly, and thoughtfully when they are used in animal patients.
Leave a comment